Ladies, let me get to the point. I want to talk today about how to look after your internal and external genitalia. It concerns me that too many girls and women do not understand how to do this. Either they have never been taught, have forgotten or have become confused by flashy marketing designed to sell feminine hygiene products (that might be doing more harm than good).
If you have a history of vaginal thrush, vulvovaginitis or bacterial vaginosis or want to avoid these problems please read on.
What makes a healthy vaginal microbiome?
You may be familiar with the gut microbiome but did you know your vagina has its own vaginal microbiome? Think of it as a beautiful garden. It needs the right environment for plants to flourish otherwise you end up with weeds.
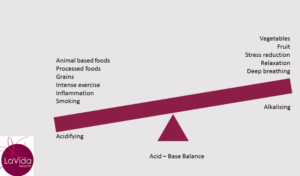
The premenopausal vaginal microbiome has a dominance of lactobacilli species including L acidophilus, L gasseri, L fermentum and others. These microbes are large producers of lactic acid meaning a healthy vagina is an acidic environment with an optimal pH of 4-4.5. Besides producing lactic acid these bugs also produce hydrogen peroxide which is vital to a healthy vagina by helping to prevent pathogen infections and keeping other microbes in balance.
There are a lot of other species in there as well but it’s the lactobacilli that are most important for good vaginal health. It’s when these are overrun by other bacteria or yeast that problems may arise.
What is vaginal dysbiosis aka vaginitis?
This occurs when the makeup of the vaginal microbiome changes in favour of a pathogenic organism i.e. the proportion of (good) lactobacilli species decreases. Common symptoms include itching, irritation, discharge and heat. Approximately 25% of cases will be due to an overgrowth of candida species (causing thrush) and a further 50% will be due to bacterial vaginosis (“BV”). Trichomoniasis (caused by a parasite) occurs in another 20% of cases.
Even if you test negative for thrush, BV or other infection it is possible that you have symptoms due to some level of dysbiosis (imbalance) of your microbiome. (Note: in postmenopausal women, it is also important to consider vaginal atrophy (thinning of the vaginal wall) as a cause of symptoms).
Risk factors for vaginal dysbiosis
There are a number of factors that may increase your risk of vaginal dysbiosis. I’m not suggesting that you stop having sex but many of these factors are well within your control, so addressing them may be very helpful. These include:
- Antibiotic use
- Hormonal changes (eg pregnancy, menopause)
- Exogenous oestrogens such as the oral contraceptive pill or HRT
- New sexual partner
- Increased sexual activity
- Smoking
- Use of intra-uterine or vaginal devices
- Use of spermicide (it’s toxic to lactobacilli)
- Vaginal washing, douching or use of bidets
- Poor toilet technique (the adjacent relationship of the vagina to the peri-anal region makes it easy for organisms to move from the rectum to the vagina)
Things to know about vaginal thrush
The symptoms of vaginal thrush (an overgrowth of yeast) are very non-specific, meaning they could be thrush or they could be something else. Sometimes there is a white vaginal discharge. Sometimes there is pain on urination or maybe an itch or perhaps swelling.
The point is, many women self-diagnose thrush and studies have shown that 2 in 3 women have got the wrong DIY diagnosis. This means, of course, that they then chose the wrong treatment and the problem doesn’t go away.
If you have symptoms, make sure you get a high vaginal swab to confirm if it is or isn’t thrush. If it is thrush, you also need to ask your doctor to establish which candida species is causing your problem. Different species require a different approach.
Approximately 80-90% of thrush cases are caused by Candida albicans and in the majority of cases will respond to “Azole” antifungals such as Canesten. However, the other 10-20% of thrush cases are caused by a different candida species (most often C. glabrata or C. tropicalis). These species are more problematic. They have a greater propensity to form a biofilm which forms a shield to protect them from the effects of OTC antifungals. So whereas these treatments will generally work in 90% of C albicans cases, this effectiveness drops to 50% in other cases and therefore a different treatment plan is required.
Vulvovaginitis (thrush) is classified as “complicated” or “uncomplicated”
Thrush will be classified as complicated in the following circumstances:
- The presence of C glabrata or C tropicalis
- If there have been recurrent infections
- If the magnitude of infection is severe
- Pregnancy
- Poorly controlled diabetes
- If there is pre-existing compromised immunity
What are the risk factors for developing thrush?
There are certain circumstances that will increase the risk of developing thrush. These include:
- Use of antibiotics
- Pregnancy
- Being immunocompromised
- Use of oral contraceptive pill or HRT containing synthetic oestrogen
Although not well understood, the presence of oestrogen seems to increase the risk of infection in some women (eg many women will report a flare-up of symptoms just prior to ovulation when oestrogen is at its peak).
What is bacterial vaginosis?
In BV we see a loss of acidity (a rise in vaginal pH to 5-6) due to the presence of bacteria (Gardnerella vaginalis) and a loss of protective lactobacilli. The common medical treatment is antibiotics which may kill the Gardnerella but also perpetuates the lack of lactobacilli leading to a high level of recurrence.
From a naturopathic perspective, there is more to treating BV than giving antibiotics. We need to change the environment of the vagina, including the acidity and restore the lactobacilli.
How to care for your vagina
There are many things you can simply do to protect your vaginal microbiome and the more prone you are to infections, the more important it is to follow these steps.
Firstly, to reduce the risk of spread of pathogens:
- Practise proper toilet technique (remember to wipe from front to back)
- Urinate before intercourse to reduce the risk of pathogens entering the vagina during intercourse
Secondly, you want to avoid excessive moisture which encourages the growth of pathogens. So:
- Don’t sit in wet bathers
- Change your underwear after strenuous (sweaty) exercise
- Use air drying after a shower
- Use loose, fresh, dry cotton underwear
- Go underwear free (eg overnight)
Thirdly, preserve your vaginal pH by doing the following:
- Urinate after intercourse (semen has a pH of 7.2-7.8) and consider post-coital rinsing* if you are particularly vulnerable to infection
- Choose your form of contraception wisely
- Don’t use soap (the average pH of soap is 7.5-9)
- Don’t use female hygiene products such as deodorisers, sprays, powders, daily panty liners or non-medicinal vaginal washes (these have all been shown to have a negative effect on pH)
How do naturopaths treat vaginal dysbiosis?
Firstly, it is important to have an accurate diagnosis. Your doctor will be able to order the appropriate swabs and tests. This is vital to the selection of an appropriate treatment plan. We want to address the underlying cause and not just the symptoms.
Our goal is to re-establish and maintain a healthy vaginal microbiome. This might include using antibacterial or antifungal herbs and nutrients along with specifically selected probiotics. Sometimes these will need to be used in conjunction with prescribed treatments (for example in C glabrata thrush).
I may recommend vaginal treatments such as pessaries or washes and I will possibly treat orally at the same time. (Given the proximity of the vagina to the rectum it may be helpful to address the gut microbiome simultaneously).
*Post-coital rinse – make up a mixture consisting of 1 part vinegar to 19 parts saline. Draw it up into a syringe and administer it to the vagina while sitting on the toilet to allow it to run back out.



2 thoughts on “How to take good care of your “lady parts””
Great article Kaye. I really enjoyed reading it.
Thank you Trisha!