Have you ever wondered about the health consequences of being on the pill?
Before my naturopathy days, I was on the oral contraceptive pill (OCP) for many years (close to two decades on and off). I didn’t have any noticeable side effects. I didn’t connect any health issues to the OCP. It was convenient to have a withdrawal bleed when it suited me. I really didn’t give it a second thought. And aside from my GP checking my blood pressure every year, I’m not sure there were any real health assessments. Certainly, I don’t recall any discussion of the risks, consequences or alternatives.
Then I did my naturopathy degree! And I began to learn about how the body works. In particular, I learnt about the many functions of hormones. Knowing what I know now, I’m confident that the pill would not have been such an automatic choice.
I believe that whether you are on the pill or thinking about it you should understand the pros and cons fully. You need to know the risks as they might apply to you, in the context of your health needs. It doesn’t matter if you are using the pill for birth control or other reasons (eg acne or period pain). There are alternatives and it may be smart to consider them before taking synthetic steroids (i.e. all forms of hormonal birth control).
What happens when you take the oral contraceptive pill?
Some people call oral contraceptives “chemical castration” as they effectively shut down your ovarian function. As a result, your ovaries stop producing oestrogen, progesterone and some DHEA and can shrink to the size of a post-menopausal woman’s ovaries (although they should recover to normal size once you cease hormonal birth control).
The form of oestrogen used in the OCP is ethinyloestradiol which is different in chemical structure to your own oestrogen. As a consequence, it has different effects in your body. Your own natural oestrogen plays a role in insulin signalling (and therefore your metabolism and regulation of blood sugar) whereas the synthetic form decreases your insulin sensitivity. This impacts your blood sugar regulation.
Depending on the form of contraception (i.e. which pill or other hormonal contraception), your progesterone is replaced with one of the synthetic forms of progestin. The most widely used of these is levonorgestrel.
As you probably know, progesterone is the pro-gestation hormone that helps to hold a pregnancy. It is also a calming hormone involved in the release of GABA. GABA is an inhibitory neurotransmitter. Without progesterone, GABA may be low, leading to symptoms of anxiety. In contrast, levonorgestrel is the same chemical used in the morning-after pill to prevent a pregnancy from taking hold. It has no calming effect and has been shown to result in increased anxiety.
More side effects of the pill
In addition to reduced insulin sensitivity and a risk of increased anxiety as mentioned above, there are other possible consequences of taking the pill.
Many of the synthetic progestins derive from testosterone and can have similar effects to testosterone in the body. This is because they have a “high androgen index”. Their side effects include:
- acne
- weight gain
- hair loss
There are hormonal birth control options with a low androgen index but they too are not without their side effects. These may include:
- suppression of adrenal function
- risk of fatal blood clots
- depression or anxiety
- loss of libido
We need our hormones, not just for reproduction, but also for a healthy brain, bone, muscles and metabolism. They are involved in the release of neurotransmitters such as serotonin and dopamine. They also influence our thyroid and adrenal functions. Unfortunately, all hormonal birth control (whether the OCP or some other form) do not use natural forms of your hormones.
Even if you don’t suffer from any of the above side effects (which are often the reason women come off birth control or at least switch to a different type), there are other consequences of hormonal birth control. These include but are not limited to:
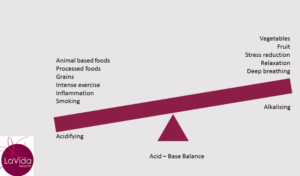
- alteration of the microbiome of the digestive tract and the vagina
- reduced bone density
- nutritional deficiencies and imbalances (particular relating to zinc and copper)
- recurrent bladder infections and thrush
A note on hair loss and the pill
Hair loss often results from hormonal birth control. The American Hair Loss Association states that hair loss will be more common on the pill if you have a family history of hair loss, so if hair loss is a concern for you, make sure you check your family history.
Hair loss will often get worse when you stop hormonal birth control. The synthetic steroid hormones cause shrinkage of the hair follicles which may take a long time to recover (if at all). If you want to know more about hair loss, please read my blog on female pattern hair loss.
What are the alternatives to the oral contraceptive pill?
If you aren’t keen to use hormonal birth control, there are some alternatives that aren’t harmful in any way, have a high (but not 100%) pregnancy prevention rate when practised correctly and allow your normal ovulatory and hormonal pattern to continue:
- fertility awareness – using temperature and symptoms to identify your fertile window
- condoms (preferably without spermicide which tends to increase the risk of bladder infections)
- femcap with contragel (a cervical cap with a non-toxic gel)
- withdrawal, particularly when combined with methods for tracking ovulation
Is an IUD better than the pill?
Another method to consider is the copper IUD. It is not without risks but the more recent ones are much safer than the earliest versions. They can result in heavy periods and pain for some women, so may not be suitable for women who already have painful, heavy periods. IUDs are best inserted by a doctor skilled in this area. Once inserted you don’t need to do anything. They have the advantage of allowing normal ovulation and are suitable for any age. The return to fertility should be rapid once removed.
A further option is the intrauterine Mirena. Its active ingredient is still levonorgestrel but as it mostly works at a local level the blood levels of this synthetic hormone are significantly lower (although some women will still experience the side effects mentioned above). It doesn’t block your normal levels of oestradiol so it doesn’t completely shut down your ovarian function although it will be reduced and you may not ovulate every cycle (in some cases up to 85% of cycles may be anovulatory in the first year). Menstrual periods will be much lighter with the Mirena and therefore it can be a good option for perimenopausal or other women who experience heavy periods.
Is hormonal birth control right for you?
If you are considering using some form of hormonal birth control I encourage you to research the side effects, risks and benefits of the particular form you are considering. I can help you with that.
Also, consider the reason why you might use these drugs and devices. Is it for contraception and if so, would other methods be safer and better for you in the long run? There is no one answer. It really depends on you and your circumstances.
If your reasons for hormonal birth control are other reasons such as acne, heavy periods, period pain or some other symptom I would encourage you to seek help to address the underlying causes of those symptoms. They are signs that something is out of balance in your system (maybe gut health or hormones) and often when we work on bringing your body back into balance, your symptoms resolve and artificial intervention is not required.
What if you are already taking the OCP?
If you are already on the OCP and you would like to come off it, I recommend you work with your naturopath. Firstly, you need to have alternative means of contraception in place. Also, we need to need to understand what your real periods were like before you went on the OCP. This will help to guide my advice regarding a treatment plan for stopping.
If prior to the OCP your periods were irregular or if you had heavy periods/pain, PCOS or acne I will commence treatment in advance of stopping the OCP. Often it is these issues that reappear when a woman stops the OCP that leave her feeling like she has no option but to go back on the pill. But there are alternatives.