Are your digestive problems or other symptoms a result of an unhealthy gut microbiome?
Your microbiome is your very own personal ecosystem made up primarily of bacteria but also includes archaea (primitive single-celled organisms), nonliving viruses, fungi and protozoa. The human microbiome refers to the genes these microbial cells harbour. It is estimated to be 75 – 200 trillion cells, considerably more than the number of cells in the human body. It’s sometimes referred to as our microbial genome, our second genome or our second brain.
The majority of your microbiome is found within the gastrointestinal system as bacteria. However there are microbial cells all over and throughout your body.
There has been an explosion of research into the constituents and role of the microbiome in the last decade. Simplistically, your microbes often get referred to as “good” or “bad” depending on what we know about that particular microbe and the role it is thought to play in your health. Whilst this holds true in a general sense, the nuances and interactions of your microbes with each other and with their host (you) are still being explored. It’s not just “what’s in there” but also the ratios of different bugs. And it is thought that the consequences of a dysbiotic microbiome (aka microbial imbalance) extend beyond the health of your digestive system into other aspects of your health.
What role does your gut microbiome play in your health?
Your microbiome has a variety of functions including:
- breaking down fibre
- digestion and liberation of nutrients (including making Vitamin K and activating Vitamin B12)
- maintaining a healthy gastrointestinal lining to prevent infections from entering your body
- supporting your immune system.
Usually, your microbiome is symbiotic, meaning the various microbial cells live in harmony with each other maintaining homeostasis (balance). Some bacteria have been identified to have benefits to your health and some have been identified to have adverse health outcomes should they be given the opportunity to flourish. You also have bacteria that enter your body through the food you eat, the water you drink, what you come in contact with and the air you breathe.
Given the right conditions your microbiome will remain fairly stable, however, having an imbalance of bacteria or proliferation of opportunistic or pathogenic bugs in your gut can lead to health complaints such as:
- Halitosis (bad breath)
- Bloating
- Burping and flatulence
- Diarrhoea
- Constipation
- Fatigue
- Increased susceptibility to illness and recurrent colds
Other conditions influenced by your gut microbiome
Research is now identifying more serious and chronic conditions that could be exacerbated or triggered by microbial dysbiosis. These include:
- Irritable bowel syndrome
- Inflammatory bowel disease (such as Crohn’s disease and ulcerative colitis)
- Atopic diseases such as eczema and asthma
- Type 1 and 2 diabetes
- Obesity
- Heart disease
- Chronic inflammation
- Various auto-immune conditions
- Mood and cognition disorders including anxiety and depression (via the gut-brain axis)
And even beyond that, it is also now understood that the diversity of our bacteria in our gut contribute to the health of other organs and body processes, such as the health of our genitourinary system (the organs of the urinary and genital systems). For example; an imbalance of gastrointestinal bacteria can influence the recurrence of urinary tract infections.
As research into the human microbiome continues we will no doubt learn more about the various communities of bacteria throughout our organs and the role they play in our health.
What causes an imbalance of microbes in your gastrointestinal system?
Medicines
One of the biggest contributors to microbial dysbiosis is the use of antibiotics. Antibiotics may of course be life-saving, however, you may also ingest antibiotics as a result of their use in farming. Not only will antibiotics alter the microbiome but excessive or inappropriate use can result in antibiotic resistance making them less effective when they are needed.
Certain other drugs such as proton pump inhibitors (eg Nexium prescribed for reflux or GORD) or pain medications can also disrupt your microbiome.
A diet high in processed foods and sugar
Processed foods offer little nutritional value and often have high amounts of sugar. Some microorganisms thrive on sugar. These opportunistic organisms, that aren’t so good for your health, can flourish.
A high level of stress or anxiety
The gut-brain axis is the two-directional pathway that links your gut to your brain. Your gut bacteria can be disrupted in times of prolonged anxiety or stress, and an imbalance of bacteria can alter neurotransmitters, having a direct effect on mood and cognition.
Excessive alcohol consumption
Alcohol changes the composition of bacteria in your gut so drinking more than two alcoholic beverages a day can have a lasting impact on your microbiome and therefore your health.
How can you keep your microbiome happy?
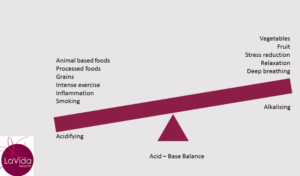
A great place to start is reducing processed and sugar-laden foods. Eat a wide variety of whole foods, lean meat and fish and lots of fruits and vegetables.
Some more specific things you can do include:
Eat prebiotic foods regularly*
Prebiotics are what feed your good bacteria so including these into your diet will ensure you are keeping your good bacteria happy. Prebiotic foods include; garlic, onion, banana, asparagus, leek, artichoke, zucchini, celery, linseeds (flaxseeds), broccoli, cabbage, kiwifruit and prunes.
Eat probiotic foods regularly*
Probiotics are live microorganisms that are found in some foods, particularly fermented foods. Probiotic sources include; yoghurt, miso, tempeh, sauerkraut, green pickles, kefir, kombucha and kimchi.
Eat foods high in resistant starch*
Resistant starch is not easily broken down by your digestive enzymes and therefore moves further down your intestinal tract and provides fuel for your good bacteria. I’ve written separately on sources of resistant starch and other fibres.
*If you find eating these foods makes your digestive health worse or you experience uncomfortable symptoms you would benefit from a consultation with your naturopath to identify the reason for your symptoms.
Drink alcohol in moderation (if at all)
Schedule at least two alcohol-free days per week and limit your alcohol on the days you drink.
Practise relaxation and or meditation
Reducing stress has a positive impact on your microbiome via the gut-brain axis so find an activity that works for you, whether that be deep breathing, meditation, painting, long walks, reading or any other pastime you find relaxing.
Are gut microbiome tests worth it?
If you’ve had digestive problems you may have been required to provide a stool sample for analysis. Generally, these tests are looking for a specific infection. They do not examine your microbiome. However, there are functional medicine tests that can provide a very comprehensive picture of your microbiome including diversity of bacteria and presence of detrimental bacteria, parasites or yeast.
These tests are sometimes extremely helpful in identifying problems, enabling us to apply a more targeted treatment strategy and monitor the effectiveness of treatments. Particularly if problems have been going on for a while and various treatments have not resolved the problem. They aren’t always necessary though. It really depends on how long you’ve had symptoms, your health history, your diet and lifestyle and other factors. I generally don’t recommend testing until a thorough assessment of your health and a discussion regarding treatment and testing options has occurred. Having said that, those of my clients who have had testing done have found it very beneficial.
A word on probiotics
Probiotics are regularly marketed for everyday use to support a healthy microbiome. There are dozens available over the counter. However; it is important to note that a broad-spectrum probiotic supplement is made up of any combination of a variety of species and strains of bacteria and therefore may not be specific to your health complaint. (It’s not unusual for a client to tell me they’ve tried a probiotic and it didn’t help).
I recommend supplementing with a broad spectrum probiotic if you have recently undergone antibiotic treatment or had “gastro”. Otherwise a consultation with your naturopath will allow for a full understanding of your current health status, and therefore ensure you are prescribed the specific probiotic strains most relevant to optimise your health.