Have you been diagnosed with endometriosis? Or do you experience symptoms that fit with endometriosis? It is a condition I see all too often in clinic. Sometimes, the effects are relatively mild but unfortunately for some, endo can be really debilitating.
What are the symptoms of endometriosis?
These will vary from woman to woman, but they may include one or more of the following:
- Painful periods
- Pelvic pain, possibly extending to your lower back or legs
- Heavy periods
- Bleeding in between periods
- Pain during sex
- Pain passing a bowel movement or whilst urinating (especially during menstruation)
- Pain during ovulation
- Lower back pain
- Fatigue
- Digestive issues such as bloating or IBS
Symptoms may come on as early as the first period (menarche) or they may develop (or get worse) during adult years. With many girls put on the pill in their teens, endo can go relatively unnoticed (and therefore undiagnosed) until you stop your contraception. In fact, it is not unusual for a diagnosis to take up to 10 years (although greater awareness is helping to bring this number down).
Occasionally, the symptoms might start as digestive discomfort which can lead to food restriction and disordered eating so it is important to have a thorough assessment to avoid this if possible.
What actually is endometriosis?
Endometriosis occurs when tissue similar to the uterus lining (endometrium) grows outside the uterus in other parts of the body. Tissue may be found on the ovaries and in the pelvic cavity, including on the bowel or bladder. The extent of tissue growth will vary from woman to woman.
Just as the uterus responds to monthly changes in your hormones, this tissue that is outside the uterus also responds to your hormonal changes. Under the influence of oestrogen, for example, the tissue thickens. However, because this displaced tissue cannot be expelled during menstruation (like the uterine lining) it continues to grow. Depending on the severity of the endometriosis, it may cause reduced fertility.
Interestingly, we used to think of endometriosis as a purely hormonal condition but research in recent years has caused us to think of it more as a disease of immune dysfunction (possibly involving the gut microbiome) triggering inflammation.
Although there is no cure for endometriosis, there are a number of treatment options available to manage the condition.
How is endometriosis diagnosed?
The only way to make a definite diagnosis of endometriosis is via laparoscopy. This is where a specialist will take a look for the offending tissue inside your pelvic cavity using a thin flexible tube with a camera attached. The specialist will also take a tissue sample to help identify it.
Other less invasive techniques may also be employed (such as ultrasound) to make a diagnosis of endometriosis and may be done in consideration of the woman’s future plans (such as planning for pregnancy).
How is endometriosis treated medically?
Treatment for endometriosis will likely depend on the severity of the condition, your age and plans for pregnancy. Often surgery is used to remove the excess tissue. This can improve your pain and fertility. Unfortunately, after surgery tissue growths may return in some women and therefore the use of hormonal medications which suppress oestrogen may be recommended. This treatment can also cause side effects so again, any treatment plan will be guided by your experience and symptoms. If you suffer from endometriosis you may already be familiar with the charity, Endometriosis Australia.
What can you do to help manage your endometriosis?
There are some great natural ways to reduce inflammation, support immune function and promote healthy oestrogen metabolism.
If you want to work on your endo, start with these tips:
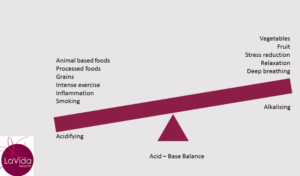
- Incorporate anti-inflammatory foods into your diet. These include turmeric, green leafy vegetables, broccoli, beetroot, walnuts, chia seeds and salmon.
- Reach for foods high in zinc to support your immune system. Try pumpkin seeds, flaxseeds (linseeds), spinach, nuts, a good quality dark chocolate (min 70%), oysters and lean beef.
- Help your body detoxify so it can metabolise and excrete excess oestrogen by including broccoli, cabbage, kale and Brussels sprouts in meals
- Exercise regularly to reduce inflammation, support your immune system, remove waste and contribute to a general sense of well-being (but avoid the high-intensity stuff and don’t overdo it)
- Avoid inflammatory foods such as those high in sugar, dairy, heavily processed or fried.
- Ensure you have good sleep practices
- Avoid plastics and other chemicals which may be adding to your inflammation
- Reduce the causes of stress in your life and make sure you incorporate some relaxation into your day.
How can a naturopath help?
I can help you with testing for possible causes of inflammation or immune dysfunction, in particular looking at your gut microbiome.
In addition to diet and lifestyle recommendations to help manage your symptoms, I use high strength herbs and supplements to reduce inflammation, modulate hormones and support the healthy lining of the gastrointestinal tract (which can support your immune system).
Before commencing any herbal or nutritional supplement, it is always wise to speak to a qualified naturopath to ensure any treatments are not only safe but appropriate for you and your symptoms.