AKA “HPA axis dysregulation”
First up I want to clarify something. Adrenal fatigue is a bit of a misnomer these days. It is a popular term to represent the effects of feeling stressed or feeling exhausted or burnt out. Sometimes it might be called “adrenal insufficiency” or “adrenal exhaustion”. It is the term most often used to describe what is now understood to be a more complex health issue.
“Adrenal fatigue” is not a recognised medical condition and it is different to primary adrenal insufficiency (aka Addison’s disease). Addison’s disease is a rare condition that occurs when the adrenal cortex (part of the adrenal gland) is damaged and fails to produce the hormone cortisol (and sometimes aldosterone). It requires medical treatment. Unlike adrenal fatigue, it is not stress-related.
So if it’s not “adrenal fatigue” what is it?
I wrote a blog a few years back entitled “Are stressed adrenals the source of your health problems?”. If you haven’t read it, I encourage you to. It explains the role of the adrenal glands and the adrenal hormones. It explains what happens when you are under stress, the myriad causes of stress and the signs and symptoms of adrenal fatigue.
While the content of that article is still relevant and I treat people with “adrenal fatigue” frequently, knowledge of human physiology continues to grow. We have refined our understanding of what is actually going on inside you (i.e. your biochemistry and how your body functions). And you guessed it, it’s not just as simple as your adrenal glands getting exhausted (like a battery going flat).
Physiological resilience and metabolic reserve
We now have a better understanding of what’s known as “physiological resilience”. That is, the capacity of a cell, tissue or organ (in this case the adrenal gland) to respond to changes in physiological need (i.e. stressors) from moment to moment. It’s our body’s ability to respond in an instant.
We also now know that each of us has a “metabolic reserve”. This is the ability of our cells, tissue or organs to withstand repeated and ongoing challenges over the long term and continue to revert to “normal” function after each challenge.
Your physiological resilience and metabolic reserve depend on your genes, diet, lifestyle and environment.
Eventually, if the challenges to your system outweigh your metabolic reserve, your system is unable to bounce back like it once did, leading to dysfunction. Your ability to return to your normal set point and resume stability of function (known as allostasis) is impaired. Your stress response remains high and your ability to cope with each new stressor diminishes.
Does this sound like you?
Do you feel like you don’t cope with stress as well as you used to?
What is happening in me?
These constant adjustments happen under the governance of the hypothalamic-pituitary-adrenal axis (HPA axis). The hypothalamus and pituitary gland (in your brain) send (and receive) signals from your organs (in this case your adrenal glands).
The HPA axis is supposed to allocate resources and influence the production of your stress hormones (amongst others). This gives you the best chance of survival in the short term (i.e. your fight or flight response). However, this comes at the expense of long term needs. This is fine provided the short term need doesn’t persist. And therein lies the problem. Constant or frequent stress results in depletion of your metabolic reserve, a loss of resilience and dysregulation of the system.
We now believe that the signs and symptoms you experience are the results of what’s happening in this bigger picture.
It starts with the signals transmitting from the brain (hypothalamus and pituitary gland) to the adrenal glands (the pathway known as the HPA axis). Maybe the signals aren’t being sent in the right amount at the right time. This perhaps explains why you are wide awake at night and sleepy all day. Or maybe they aren’t being received…a bit like when you talk to your kids or partner and they don’t seem to hear you despite having perfectly good hearing.
This could be the problem with your adrenal glands….they are capable of working but they aren’t picking up the signals.
So “adrenal fatigue” or “adrenal exhaustion” are more accurately referred to as
HPA axis dysregulation.
What are the long term effects of not addressing HPA axis dysregulation?
The adrenal glands play a major role in a number of body systems. The impact of leaving this dysregulation unaddressed may increase your risk of:
- Cardiovascular disease
- Chronic fatigue syndrome
- Insulin resistance and hypoglycaemia
- Thyroid dysfunction
- Recurrent and chronic infections
- High or low blood pressure
How do we treat adrenal fatigue or HPA axis dysregulation?
As you have gathered by now, the best approach is to look at your whole system and not just focus on the adrenal glands.
We need to rule out other possible causes of your symptoms. These might include (amongst other things):
- Addison’s disease
- Hypothyroidism
- Anaemia
- Hypoglycemia
- Autoimmune diseases
- Depression
- Gut dysbiosis, infection or bacterial overgrowth
Importantly for you, this enhanced understanding has given naturopaths and functional medicine practitioners greater scope to hone our treatment plans. Are the adrenal glands struggling to produce hormones or are they not getting the instruction to do so? Do we need to work on supporting metabolic reserve by better understanding the intricate relationship between your genes, diet, lifestyle and environment?
Sometimes, testing of adrenal function (generally by testing adrenal hormones in the saliva, blood or urinary metabolites) can be beneficial but it is important to understand the context. Low cortisol may not necessarily mean that the adrenal glands can’t produce cortisol (as is often thought). It may actually reflect a down-regulation of the HPA axis in order to protect tissues in the body from too much cortisol. A test showing low cortisol is not necessarily reflective of the adrenal gland’s ability to produce cortisol.
The production of stress hormones will also be influenced by the brain’s perception of stress. Is it new stress or have you seen it before? Do you have any sense of control? Is it unpredictable? Are there any imbalances in neurotransmitters such as glutamate, dopamine or serotonin which may affect how you feel in response to a stressor?
What should you do if you suspect that you have adrenal fatigue or HPA dysregulation?
Your GP is a good place to start (and most people have already been to their GP before they come to see me). Remember that your GP may not acknowledge the term “adrenal fatigue” or even HPA axis dysregulation but describing your symptoms in detail (using the list outlined in my early blog) should give them enough information to run some initial tests to consider possible causes.
Then make an appointment with a good naturopath and bring your pathology results. We will make a thorough health assessment and develop a plan of attack. This may include functional pathology testing, dietary and lifestyle assessment.
Once we have established the likely underlying cause of your symptoms, usually changes to diet and lifestyle will be incorporated into a detailed treatment plan along with nutritional and herbal supplements.
Some of the key areas to focus on will be:
Sleep – good quality sleep for 7-8 hours is one of the best ways to reset your HPA axis
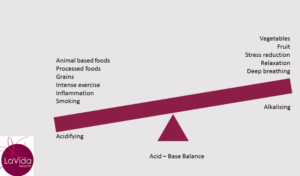
Inflammation – this is a key stressor and disruptor of your HPA axis. We need to find and address the source of your inflammation (e.g. infection, toxic load, excess body fat, disrupted gut microbiome, poor digestion)
In the meantime, to help nourish your adrenal glands ensure you are eating nutrient-dense foods high in vitamin C, the B vitamins and magnesium. Foods that contain these nutrients include berries, citrus fruits, broccoli, avocado, leafy green vegetables, nuts and seeds and eggs. Make sure you also include lean protein in your diet.
And don’t forget to practice some relaxation. Deep breathing, yoga, meditation and even laughter are all fabulous for switching you out of that ‘constantly stressed’ state and giving your HPA axis some much-needed balance.