Ladies, your period should be largely pain-free, come at regular intervals and should not be excessively heavy. And it should almost catch you by surprise due to a lack of premenstrual symptoms.
In other words your period should not disrupt your life and you shouldn’t have to plan your days around your cycle.
What are some of the menstrual problems you might encounter?
Unfortunately, too many women have issues with their menstrual cycle. So much so that they think it is normal because most of their female friends or family suffer as well. They think their pain is something they just have to put up with. Or they believe the only solution to their problems is to go on the contraceptive pill.
Here are some of the more common problems women face with their periods.
Premenstrual syndrome/symptoms (PMS)
It is estimated that approximately 1 in 3 women suffers from severe PMS. In some cases, enough to incapacitate them for days every cycle. And as I said at the start, your period should almost arrive by surprise. A week or more of warning signs is your body’s way of telling you something is not quite right.
PMS symptoms generally start a couple of days before your period. But some women experience PMS for the entire second half of their cycle (after ovulation). They usually dissipate within a day or so of your period starting.
PMS may include one or more of the following symptoms:
Mood changes are the most frequently reported symptoms in my clinic. Specifically, this can present as grumpiness, irritability, anger, anxiety, a short fuse or impatience. Or maybe you become more emotional or depressed, bursting into tears or feeling overwhelmed at the drop of a hat.
Bloating, fluid retention or sore breasts are other common symptoms. Some women will go up a dress size for a week or more every month.
Acne flares or breakouts are often due to premenstrual hormonal changes but can also be exacerbated by inflammation and diet.
Cravings for certain foods…chocolate and cakes seem to be particularly popular.
Pain in the abdomen or lower pelvic region or pain in the form of pre-menstrual migraines
Brain fog or forgetfulness
Insomnia and fatigue which can exacerbate mood changes, cravings and cognition
Painful periods (aka dysmenorrhea)
The majority of women will experience some period pain with their bleed. The fortunate ones experience only mild discomfort in the hours leading up to the commencement of their bleed and then perhaps for a few more hours. However, others will have pain so severe that they are bed-bound for days with heat packs and analgesics providing only limited relief.
The types of pain can vary. Pain may be in the form of a dull ache or perhaps a sense of dragging and fullness. It could also be in the form of griping, cramp-like pain. Generally, pain is in the lower abdomen but sometimes women will experience lower back pain and even pain extending down the legs.
There are two different classifications of dysmenorrhea. Secondary dysmenorrhea is period pain that is the result of an underlying condition such as endometriosis. Endometriosis is thought to affect 1 in 10 women. The other classification for painful periods is called primary dysmenorrhea. This is the term given to period pain where there is no identified underlying condition.
Heavy periods (aka menorrhagia)
For most women, their period lasts between 3 and 7 days with some of these days having only some light spotting. The average loss of blood is approximately 50ml and for these women, there is no particular impact on daily activity or nightly sleep. Generally, they only need to change a regular tampon or pad every couple of hours on the “heavier” days. They can get through the night uninterrupted as their flow generally slows overnight.
However, many women experience menorrhagia or heavy periods. Your period is considered to be heavy if you lose more than 80ml of menstrual fluid. (Some women may even losing up to 500ml in rare circumstances). As a guide, a regular, soaked tampon holds approximately 5ml so 80ml of menstrual fluid would fill 16 regular tampons.
Heavy periods may be the result of an underlying condition such as the presence of a fibroid. Other causes may include hormonal imbalances, thyroid problems or low iron levels.
Irregular periods
A typical healthy cycle results in a period approximately every 28 days (but your “regular” could be anything from 21 to 35 days. The point is that it is regular and predictable.
An irregular period is one that is unpredictable. You might have a 28-day cycle one month followed by a 45-day cycle the next or maybe it’s a 16-day cycle. There just doesn’t seem to be any predictable pattern to it or it falls outside the norm (eg predictably every 45-50 days).
There are many possible reasons for irregular periods. They may be the result of anovulatory cycles (i.e. you didn’t ovulate that month) or hormonal imbalances. An underlying condition like Polycystic Ovarian Syndrome (PCOS) (which is estimated to affect up to 15% of women) could also be the problem. And eve increased stress can disrupt a cycle.
I’ve written in greater depth about irregular cycles in a separate blog.
Transition to menopause
Perimenopause is the time leading up to your last period (menopause). It will most often start in your mid-late 40s but can start earlier.
This is a time of fluctuating hormones that can result in significant changes to your “normal” menstrual cycle. Your cycle can fluctuate in length, get heavier or more painful and you may experience hot flushes or increased PMS-type symptoms. If you want to know more about this time in a woman’s life read about the pesky perimenopause.
What’s causing your menstrual problems?
There are many causes or triggers of all these menstrual problems and sometimes it might be a combination of more than one thing (a perfect storm).
In my clinic, I often see women who have been put on the pill in their teen years when their problems started. The pill masks the problem, then they come off the pill in their 20s or 30s only to find that the symptoms return with a vengeance. Unfortunately, unless they address the underlying causes the symptoms will likely remain until menopause.
So, what are the common drivers?
Imbalance of key sex hormones
Your sex hormones (primarily oestrogen and progesterone in this instance) should be made on-demand, in varying amounts throughout your menstrual cycle. Once they have served their purpose for that month your body breaks them down and eliminates them (i.e. detoxification and elimination).
Oestrogen’s primary job is to aid ovulation and prepare the uterus to receive a fertilised egg. Beyond fertility, oestrogen is also important for healthy bones and muscles, cardiovascular health, brain function, sleep and metabolism. But you can have too much of a good thing. Oestrogen may also promote inflammation and growth. We see the symptoms of fibroids and endometriosis as worsening under the inflammatory effects of too much oestrogen. This is especially the case when our body’s own detoxification processes are slow to remove unwanted oestrogen.
Progesterone is made during the second half of your cycle if you have ovulated. Besides preparing your uterus for the possible arrival of a fertilised egg, progesterone also performs many vital functions. It has a calming effect on your mind, helping with mood and sleep. It is also anti-inflammatory.
If you have not ovulated you won’t make progesterone. Even if you have ovulated sometimes your progesterone levels are insufficient to achieve the desired calming effect or perhaps other hormonal changes can interfere with its function.
Other hormones
Your hormones should not be looked at in isolation. They all interact with each other like a beautiful, harmonious orchestra playing in perfect tune and sync. But it only takes one “instrument” to be slightly off-time or out of tune to throw out the whole sound and instead of beautiful music you just have “noise”.
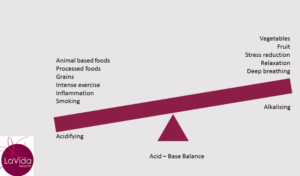
Elevated blood glucose due to dysfunction in the hormone insulin may lead to increased inflammation which can affect oestrogen and testosterone production and exacerbate inflammatory conditions.
Increased stress in your life results in the increased production of the stress hormone, cortisol. Cortisol is made from many of the same ingredients (called precursors) as your sex hormones. In times of stress, your body will prioritise cortisol over your sex hormones. (As well as the hormonal effects, stress may also impact your temperature regulation, making you more prone to hot flushes or chills).
Problems with thyroid function (especially hypothyroidism) affect the production of thyroid hormones which can interfere with progesterone, resulting in increased PMS symptoms or irregular periods. (And hypothyroidism may also contribute to poor digestion and detoxification).
Detoxification and elimination
Inadequate detoxification (by the liver) can result in poor clearance of hormones leading to accumulation of excess hormones (particularly oestrogen) which may be the underlying cause of heavy periods, fibroid growth or endometriosis.
Dysbiosis or an imbalance of bacteria (our microbiome) in the digestive tract can affect detoxification and elimination of waste (including toxins) and can lead to inflammation.
Other factors that can affect your digestive processes include alcohol, some pharmaceutical medications, stress and a diet lacking in vital nutrients.
Inflammation underlies many menstrual cycle problems
Inflammation may interfere with hormone regulation and function. In some circumstances, it may prevent ovulation (and so contribute to low progesterone).
There are many possible causes of inflammation. I’ve already mentioned some of these but another common cause is carrying a bit too much adipose tissue (i.e. fat) around your abdomen. This particular type of fat is known to promote inflammation and oestrogen production.
An overload of toxins coming from your diet or environment
I’ve written elsewhere about the role of toxins in our health but I want to make specific mention of particular toxins called “endocrine-disrupting chemicals” (EDCs). There are numerous studies linking these chemicals to problems of hormonal dysfunction in both males and females. EDCs may be found in plastics, cleaning products, personal care products, some food additives and certain pesticides.
These are all triggers that can be reduced with simple treatments and diet or lifestyle changes.
There’s no need to suffer in silence.
The naturopathic approach to fixing your menstrual cycle problems
In rectifying your menstrual problems, be prepared for it to take a few cycles. Hormones are cyclical in nature and it takes some time to establish your new rhythm.
My naturopathic approach is to provide symptomatic relief through targeted nutritional and herbal remedies specifically chosen to address your individual symptom picture. There are lots of tools in my tool kit. Specific nutrients and herbs are wonderful for addressing pain, heavy flow, mood issues, cravings and more.
While doing this, we also seek to address all the underlying drivers of your symptoms. This depends on what is happening for you. It might include working on your detoxification and elimination pathways or balancing hormones. It might be reducing inflammation and addressing its causes. We may also work on reducing stress and improving your resilience, all the while ensuring your diet and lifestyle are supportive of a healthy hormonal balance.